
TTTREE – Trauma Trigger Therapy

What is Trauma informed CPTSD Therapy
Trauma informed therapy helps you to understand relational and interpersonal dynamics exploring how trauma impacts perceptions and how interactions and relationships with others can cause trauma triggers.
Trauma focused relational therapy can help individuals navigate, process and alter the triggered reaction by empowering them to explore alternative response styles raising awareness of their fight and flight behaviours.
CPTSD (Complex Post-Traumatic Stress Disorder) trauma triggers are specific stimuli that can evoke intense emotional and physical responses or sensations that reflect the individual’s earlier childhood trauma. These triggers can vary widely from person to person but commonly include:
1. Sensory Triggers.
Certain sounds, smells, or sights that remind an individual of the traumatic experience can provoke strong emotional reactions. For example, the sound of a siren or a particular song.
2. Emotional Triggers. Situations that evoke feelings of helplessness, fear, or abandonment can trigger trauma responses. This might include conflicts or situations that feel overwhelming. When encountering a trigger, individuals may experience a surge of anxiety, panic attacks, muscle tension, chest pain, dizziness, rapid heartbeat, shallow breathing, sweating, nausea, stomach aches, crying, shaking, feeling disorientated, emotional numbness, irritability or anger, dissociation or avoidance behaviours.
3. Situational Triggers. Being in specific environments or situations that resemble the traumatic event can cause distress. For instance, visiting a location where trauma occurred or encountering a similar setting.
4. Interpersonal Triggers. Interactions with certain people or types of relationships (like authority figures or individuals who exhibit controlling behaviour) can evoke feelings of fear or anxiety.
5. Physical Triggers. Physical sensations, such as pain, fatigue, or feelings of being trapped, can remind someone of their trauma and trigger distress.
6. Anniversaries or Reminders. Dates or events that coincide with the traumatic experience (such as anniversaries of loss or significant dates) can trigger memories and emotions related to the trauma.
7. Media Exposure. News stories, movies, or shows depicting similar traumatic events can evoke memories and feelings associated with past trauma.
8. Changes in Routine. Disruptions in daily life or unexpected changes can trigger anxiety or feelings of instability, reminding individuals of their trauma.
9. Isolation or Loneliness. Feelings of being alone or disconnected can trigger memories of past abandonment or neglect.
10. Substance Use. The use of alcohol or drugs can sometimes trigger memories or feelings related to past trauma, leading to heightened emotional responses.
Understanding these triggers can help individuals develop coping strategies and seek
appropriate support to manage their reactions effectively.
While some trigger points for trauma may be universal, such as reminders of violence, loss, or abandonment, individual reactions to these triggers can vary significantly.
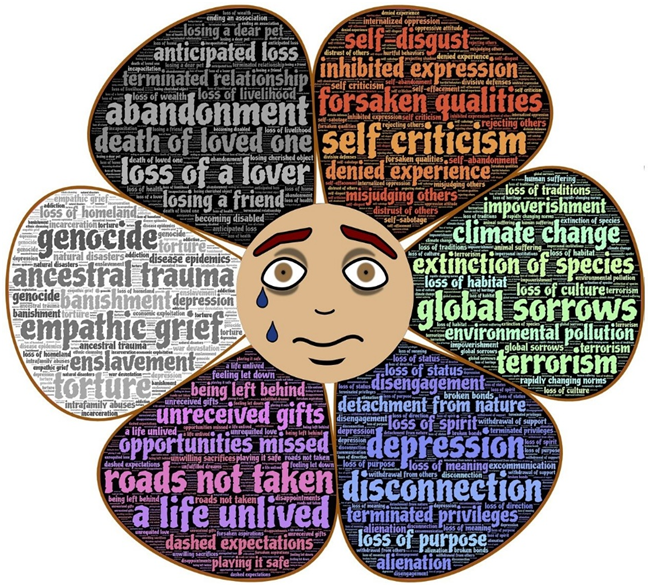
Other deeper rooted triggers could be:-
1. Universal Triggers. Certain experiences tend to evoke strong reactions across many individuals, such as sounds associated with danger (e.g., shouting, sirens), specific smells (like smoke), or visual reminders of traumatic events. These triggers can provoke feelings of anxiety or distress in a wide range of people.
2.Individual Reactions. Each person’s background, personality, and coping mechanisms influence how they respond to triggers. For example, one person may become visibly agitated when confronted with a trigger, while another might withdraw or become emotionally numb.
3. Personal History. A person’s unique experiences and history shape their trigger points. Someone who has experienced loss may react strongly to reminders of that loss, while another individual might have a different association with the same trigger based on their personal narrative.
4. Cultural Influences. Cultural background plays a significant role in shaping perceptions of trauma and triggers. Different cultures may have varying beliefs about mental health, emotional expression, and coping strategies, affecting how individuals respond to trauma-related stimuli.
5. Coping Strategies. People develop different coping strategies based on their experiences. Some may use healthy coping mechanisms like seeking support, while others might resort to avoidance or substance use, leading to diverse reactions when faced with triggers
6.Contextual Factors. The context in which a trigger occurs can also influence the reaction. A person may feel safe and supported in one environment but overwhelmed in another, leading to different responses to the same trigger.
7. Emotional Regulation. Individuals vary in their ability to regulate emotions. Some may manage their feelings effectively, while others may struggle, resulting in heightened reactions when triggered.
8. Support Systems. Access to supportive relationships and resources can impact how someone responds to triggers. A strong support network can help individuals navigate their reactions more effectively.
9. Awareness and Insight. Individuals who have a deeper understanding of their trauma and triggers may handle them better than those who are unaware of their emotional responses.
10. Healing Journey.The healing process is unique for everyone. As individuals work through their trauma, their reactions to triggers may evolve, potentially becoming less intense over time.
Recognizing the complexity of trauma triggers and individual responses is essential for fostering empathy and providing appropriate support to those navigating their healing journeys.
Everyone has unique trigger points. Some people can trigger us without having to do any of the actions on the list.
Our reaction to a trigger is somatic and are often felt powerfully and manifest physically in the body.
Our responses to trauma triggers are more profound than any cognitive understanding. This somatic reaction can involve various physiological responses, including increased heart rate, muscle tension, or changes in breathing patterns, all linked to our nervous system’s activation.
Somatic Experience and the Nervous System
When we encounter a trigger, our nervous system can shift into a state of heightened alertness, often referred to as the “fight or flight” response. This physiological reaction is rooted in our body’s instinctual survival mechanisms. For example:
Increased Heart Rate. You might notice your heart racing when recalling a distressing memory, signaling your body’s readiness to respond to perceived danger.
Muscle Tension. Feelings of anxiety or fear can lead to tightness in your shoulders or neck, as your body braces itself against potential threats.
Shallow Breathing. A sense of panic may cause you to breathe more rapidly or shallowly, which can further heighten feelings of anxiety.
Somatic Exercises for Awareness Tracking and Pendulation
1. Awareness Tracking Exercise
Find a Comfortable Position. Sit or lie down in a comfortable position, ensuring you feel supported.
Breathe Deeply. Close your eyes and take several slow, deep breaths, allowing your abdomen to expand fully with each inhale and contract with each exhale.
Body Scan. Gradually bring your awareness to different parts of your body, starting from your toes and moving up to your head. Notice any sensations, areas of tension, or discomfort without judgment.
Label Sensations. As you scan, label the sensations you feel (e.g., tightness, warmth, heaviness) and observe how they shift as you continue to breathe.
Pendulation is a concept primarily used in somatic therapies, particularly in the context of trauma healing. It refers to the natural rhythm of moving between states of tension and relaxation, or between activation and calmness, in response to traumatic experiences. This process helps individuals to gradually process and integrate traumatic memories and sensations without becoming overwhelmed.
Here’s a deeper look at pendulation:
1. Natural Rhythm. Pendulation acknowledges that human experience often involves fluctuations between different emotional and physical states. Just as a pendulum swings back and forth, individuals can oscillate between feeling activated (e.g., anxious, fearful) and feeling relaxed or grounded.
2. Trauma Processing. In the context of trauma, pendulation allows individuals to approach their traumatic memories or sensations in a manageable way. Instead of diving headfirst into the trauma, they can briefly engage with the difficult emotions or physical sensations, then return to a state of safety and calmness.
3. Building Resilience. By practicing pendulation, individuals can build resilience and develop a greater tolerance for discomfort. This gradual exposure helps them to process trauma without becoming overwhelmed, making it easier to integrate their experiences over time.
4. Mind-Body Connection. Pendulation emphasizes the importance of the mind-body connection in healing. It encourages individuals to be aware of their physical sensations and emotional states, allowing them to recognize when they are feeling activated or relaxed. This awareness can empower them to navigate their feelings more effectively.
5. Therapeutic Application. In therapeutic settings, practitioners may guide clients through exercises that facilitate pendulation. This might involve focusing on a painful memory for a short period, then shifting attention to a positive memory or engaging in grounding techniques to promote relaxation.
6. Safety and Control. Pendulation helps create a sense of safety and control in the healing process. By allowing individuals to move back and forth between discomfort and comfort, it fosters a sense of agency over their healing journey.
Overall, pendulation is a valuable concept in trauma therapy, helping individuals to process their experiences in a balanced and manageable way, ultimately leading to greater healing and integration.
2. Pendulation Exercise.
Try this technique to identify a trigger
Identify a Trigger. Think of a recent situation that triggered a strong emotional or physical response. Notice where in your body you feel the most tension or discomfort related to this trigger.
Shift Attention. Gently shift your focus away from the discomfort to a neutral or pleasant sensation in your body. This could be the feeling of your feet on the ground, a gentle breeze on your skin, or warmth in your hands.
Alternating Focus. Alternate your focus between the discomfort (the trigger) and the pleasant sensation (the resource) for a few minutes. This process, known as pendulation, helps to regulate your nervous system by creating a balance between activation and calm.
Integrate the Experience. After several cycles, take a moment to reflect on how your body feels. Notice any changes in tension or discomfort, and consciously acknowledge the shift.
These somatic practices can enhance your awareness of bodily sensations and help you develop a deeper understanding of how your body reacts to triggers. By learning to navigate these experiences, you can foster resilience and promote healing within your nervous system.
10 common beliefs people may have during a panic attack
1. “I’m going to die.”
2. “I’m losing my mind.”
3. “I can’t breathe.”
4. “I’m going to embarrass myself.”
5. “I have no control over my body.”
6. “This feeling will never end.”
7. “Something terrible is about to happen.”
8. “I’m weak for feeling this way.”
9. “I can’t handle this.”
10. “I’m completely alone in this”
Try Reframing these Statementsto:-
1. “This 1. feeling is intense, but I am not in danger.”
2. “I am experiencing panic, but I am still in control.”3. “I can focus on my breathing; I have the ability to calm myself.”
4. “It’s okay to feel anxious; many people experience this.”
5. “I can ground myself and regain control over my body.”
6. “Panic attacks are temporary; this will pass.”
7. “I can manage this moment by using my coping skills.”
8. “Feeling anxious doesn’t define my strength or worth.”
9. “I have handled panic before, and I can do it again.”
10. “I can reach out for support; I am not alone.”
These reframing statements can help individuals challenge their negative thoughts during a panic attack and cultivate a more balanced and supportive mindset.
10 supportive statements you can say to someone who is experiencing a panic attack or intense anxiety:
1. “I’m here for you.” This reassures them that they are not alone and that you are present to support them.
2. “It’s okay to feel this way.” Validating their feelings can help reduce shame or fear about their experience.
3. “Take your time; there’s no rush.” Encouraging them to take their time can help relieve pressure and allow them to focus on calming down.
4. “Let’s focus on your breathing together. “Suggesting a breathing exercise can help them regain control and ground themselves.
5. “What can I do to help you right now?” Helping empowers them to express their needs and preferences.
6. “You’re safe here.” Reassuring them of their safety can help alleviate feelings of panic and fear.
7. “This feeling will pass.” Reminding them that panic attacks are temporary can help them see the light at the end of the tunnel.
8. “Can we find a quiet place to sit?” Suggesting a change of environment can help them feel more comfortable and less overwhelmed.
9. “I believe in you; you can get through this. “Expressing confidence in their ability to cope can provide encouragement and strength.
10. “Let’s take a moment to focus on something around us. Prompting them to engage their senses can help divert their attention from the panic and ground them in the present.
These statements can provide comfort and support, helping the individual feel understood and less alone during a challenging moment.
Dissociation.
When exploring trauma triggers, it’s essential to be cautious if you or anyone your supporting experiences dissociation. This state can create a disconnection from your thoughts, feelings, or sense of self, making it difficult to process emotions effectively. Diving into triggers without proper grounding can lead to overwhelming feelings and exacerbate feelings of confusion or detachment, hindering your healing journey.
Taking a mindful approach can help you navigate these experiences safely. Establishing a supportive environment, using grounding techniques, and knowing when to pause or seek assistance can prevent further distress.
Remember, it’s okay to take your time and prioritize your emotional well-being as you work through trauma triggers.
Dissociation, depersonalization, and derealization are psychological phenomena that can occur as coping mechanisms in response to trauma, stress, or overwhelming emotions. Here’s an explanation of each, along with coaching and therapy guidance for those who experience these sensations.

Dissociation. This is a mental process where a person disconnects from their thoughts, feelings, memories, or sense of identity. It can manifest to cope with trauma or stress, allowing individuals to detach from painful experiences.
Depersonalization. This specific type of dissociation involves feeling detached from one’s body or sense of self. Individuals may feel as if they are observing themselves from outside their bodies or as if they are not real.
Derealization. This involves a feeling of detachment from the external world. Individuals may perceive their surroundings as unreal, dreamlike, or distorted, leading to a sense of disconnection from reality.
Why They Happen? They often arise in response to:
Trauma. Experiencing traumatic events can lead to dissociation as a protective mechanism to help individuals cope with overwhelming emotions or memories.
Stress. High levels of stress or anxiety can trigger dissociative symptoms, serving as a way to escape from distressing situations.
Emotional Overload. When emotions become too intense, dissociation can provide temporary relief, allowing individuals to distance themselves from their feelings.
Coping mechanisms. Some individuals may have learned to dissociate to handle challenging emotions or situations throughout their lives.
Books on Trauma and Triggers:
The Body Keeps the Score, by Bessel van der Kolk.
This book explores how trauma affects both body and mind, providing insights into healing processes.
Waking the Tiger. Healing Trauma by Peter A. Levine
Levine offers a new perspective on trauma and how to work through it by understanding it as a natural response to overwhelming experiences.
The Trauma Recovery Workbook.A Guide to Healing from Trauma, by Susan Pease Banitt
This workbook provides practical exercises and insights for individuals recovering from trauma.
Complex PTSD: From Surviving to Thriving” by Pete Walker**: Walker discusses the symptoms of Complex PTSD and offers strategies for healing and recovery.
The Deepest Well: Healing the Long-Term Effects of Childhood Adversity. by Nadine Burke Harris.
This book examines how childhood trauma impacts health and well-being and provides insights into healing.
Healing Trauma: A Pioneering Program for Restoring the Wisdom of Your Body by Peter A. Levine and Ann Frederick.
This guide offers practical techniques to help individuals heal from trauma.
The Emotionally Abusive Relationship” by Beverly Engel.
Engel explores the impact of emotional abuse and trauma, including triggers and healing strategies.
It Didn’t Start with You. How Inherited Family Trauma Shapes Who We Are and How to End the Cycle” by Mark Wolynn.
This book delves into the concept of inherited trauma and its effects on individual lives.
These books provide valuable insights into understanding trauma triggers and the healing process, offering guidance for those navigating their own experiences.
For more interesting blog articles about trauma healing, recovery and mental health tips visit my linkeden page follow me Heline Freea.
© 2025 Heline Freea. All rights reserved.
